Substance Use Disorders Impact on Rural America
Substance Use Disorders Impact on Rural America
Though often perceived to be a problem in highly populated urban areas, the rise of substance use disorders (SUDs) has increased substantially in small towns and rural areas throughout America over the past 20 years.
Updated: 2023
Written by: Allendale Treatment
If you or anyone you know are struggling with addiction, call (833) 338-6946 to speak with a professional.
In March 2021, the Centers for Disease Control and Prevention (CDC) noted that while drug overdose death rates continued to rise in both rural and urban areas – in states like California, Connecticut, North Carolina, Vermont, and Virginia, the rate of drug-overdose deaths in rural counties were higher than in urban ones.
In addition, rural communities that have strong coal, lumber, farming and manufacturing industries have been targeted by pharmaceutical companies since the 1990s with misleading advertising about pain-reducing prescriptions that fueled the opioid epidemic. A survey by The National Farmers Union and the American Farm Bureau Federation reported that 74 percent of farmers said they were directly impacted by the opioid crisis. Lack of access to treatment, economic issues and other unique challenges are also contributing factors to the increase of substance use disorders throughout rural America.
Rural Counties Struggle with the Ongoing Impact of the Opioid Epidemic
Research indicates that states with large rural populations have some of the highest rates of opioid prescriptions. Drug overdose deaths involving prescription opioids rose 376 percent from 3,442 in 1999 to 16,416 in 2020. As lawmakers in these areas passed legislation to reduce the number of people abusing painkillers, many people who were addicted turned to illegally purchasing heroin, methamphetamines and fentanyl when they were no longer able to get their prescriptions.
In the Rural Opioid Initiative study led by Dr. Todd Korthuis, director of the Addiction Medicine Section at Oregon Health & Science University, in Portland, Korthuis and his colleagues found that most of the participants were using methamphetamines without realizing that most of them were laced with fentanyl.
“Methamphetamine is increasingly contaminated or adulterated with fentanyl, which is 50 to 100 times more potent than heroin,” says Korthuis.
Drinking Culture Driving Alcohol Abuse in Rural Areas
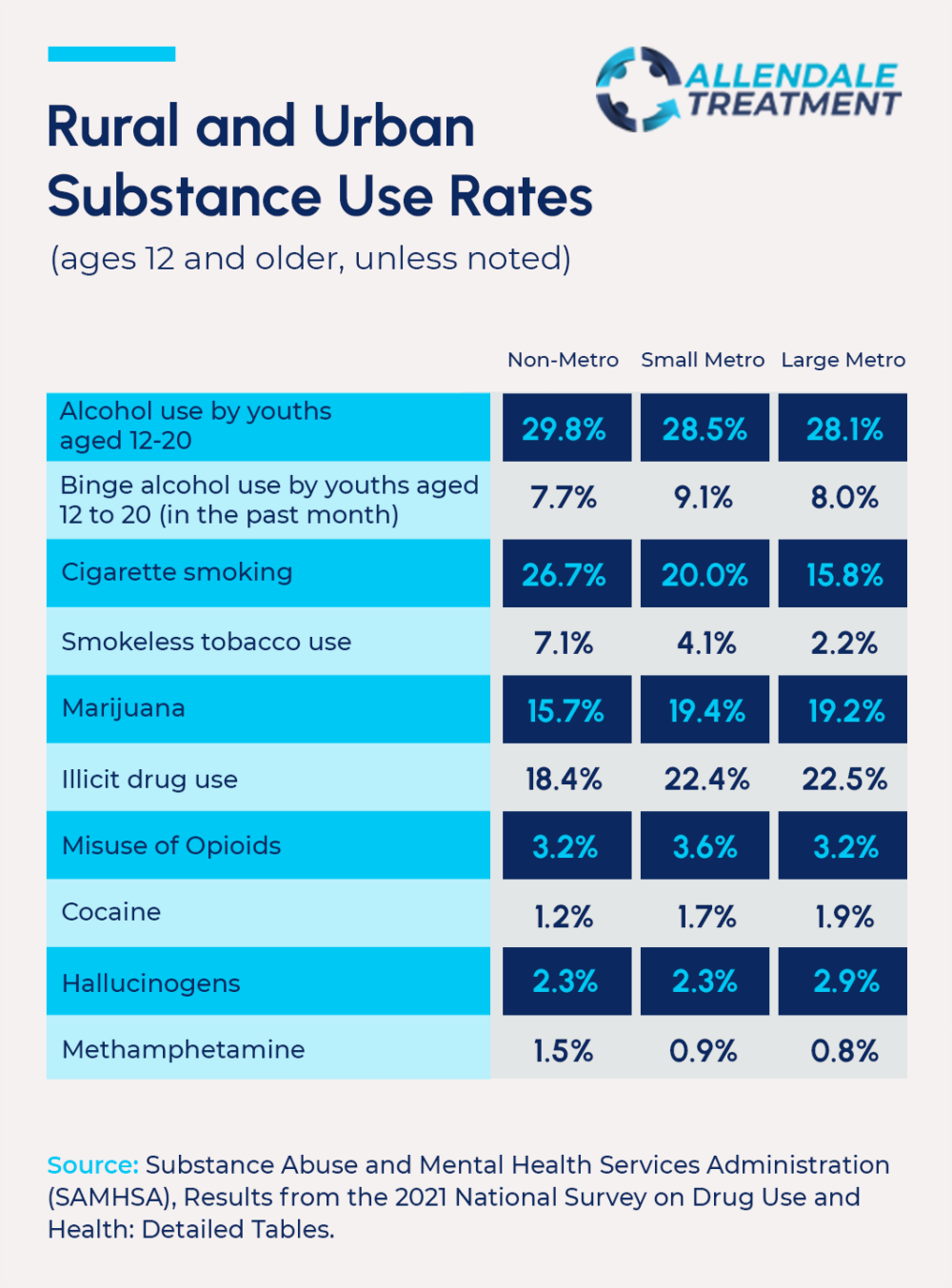
According to data from the 2021 National Survey on Drug Use and Health alcohol use among 12 to 20-year-olds was higher in nonmetro areas compared to large metro areas including binge drinking and the CDC reported that alcohol-related deaths increased by 26% from 2019 to 2020. Jennifer Husmann, a project coordinator with the Iowa Area Substance Abuse Council, says that’s certainly the case in rural Iowa where nearly 850 people have died of alcohol-related causes in the council’s latest count.
Husmann says that alcohol abuse is a serious concern in rural Iowa, where driving under the influence of alcohol continues to climb – causing traffic-related fatalities and health issues. She says that access to alcohol has also gotten easier which has further exacerbated the issue. “We now have hard liquors, spirits available in every gas station, and convenience store in Iowa,” said Husmann. “It’s easier to find alcohol-flavored whiskey in little tiny towns sometimes than it is to find an apple. We don’t think about how dangerous alcohol really is and how many people are dying. It’s enough people to fill Wrigley stadium one and a half times.”
A study from the Maine Rural Health Research Center, suggests that rural adolescents reported higher rates of driving under the influence than urban adolescents and several factors may be contributing to this risky behavior including:
Rural Communities Face Unique Challenges Addressing Substance Abuse
Substance use disorders within a rural community can present many problems including increased crime, vehicle accidents caused by impaired driving, homelessness and unemployment. These problems are compounded by several unique challenges in rural communities including:
People in rural settings may also be hesitant to seek treatment because they are afraid of facing possible ostracization or isolation. Tommy Streeter, a community outreach coordinator for Allendale Treatment and Fort Wayne Recovery grew up in a community located in rural Indiana and says that one of the fears he faced when starting his recovery was losing his group of friends.
“A common fear people have in rural areas is losing their friends because they won’t be able to join them at the local bar or get high with them,” says Streeter.
Rural Communities Look for News Ways to Expand Access to Treatment
With more than 50% of all rural counties lacking a Drug Enforcement Administration-waivered medication-assisted therapy (MAT) provider, and almost 30% of rural Americans living in a county without a buprenorphine provider, rural communities are looking for new ways to provide drug and alcohol prevention and reduction services.
Andrea Storjohann is a nurse practitioner in Iowa who prescribes buprenorphine, a MAT, to dozens of patients who have become addicted to heroin or opioid painkillers. She works at a general-practice clinic in central Iowa that focuses on creating privacy for its patients by showing no signs of it being a place for people to seek treatment for a SUD. “You could be coming here for OB-GYN care. You could be coming here for a sore throat. You could be coming here for any number of reasons, and no one in the waiting room would know the difference,” says Storjohann. “We were kind of a unicorn in this part of the state,” but according to a University of Washington study that’s changing. In 2016, just 40% of rural counties in the United States had at least one healthcare provider certified to prescribe buprenorphine but that figure climbed to 63% by 2020.
The recently announced federal funding is also providing hope to rural communities who would like to use the funds to build more treatment centers, expand MAT and NARCAN accessibility and hire more medical practitioners and behavioral health specialists for their small towns, “I think one of the biggest things when it comes to treatment is what types of treatments are available and of those types of treatments, what is going to best suit somebody?” said Patrick Habecker with the University of Nebraska Lincoln’s Rural Drug Addiction Research Center.
Habecker explains that In Omaha, there are 119 facilities listed in a 100-mile radius compared to North Platte where there are only 12 in a 100-mile radius. “When you’re outside of Lincoln, Omaha, Grand Island even, to what extent is it easy to drive 10 miles, 20 miles, to have to spend an hour in a vehicle regularly to sort of get this treatment?”
He also believes that it’s important for people no matter where they live to have easy access to substance use treatment facilities and programs to combat addiction throughout the country. “When that moment arrives when someone is looking to reduce or change how they use a substance or completely remove it, you want as few barriers as possible there. You want to make that an easy transition where the services are available, easy to access and they’re not going to face a whole bunch of stigma for walking in the door.”
If you or anyone you know are struggling with addiction, call (833) 338-6946 to speak with a professional.

