Better Access to Mental Health Services Could Reduce Substance Use Disorders and Overdoses
Better Access to Mental Health Services Could Reduce Substance Use Disorders and Overdoses
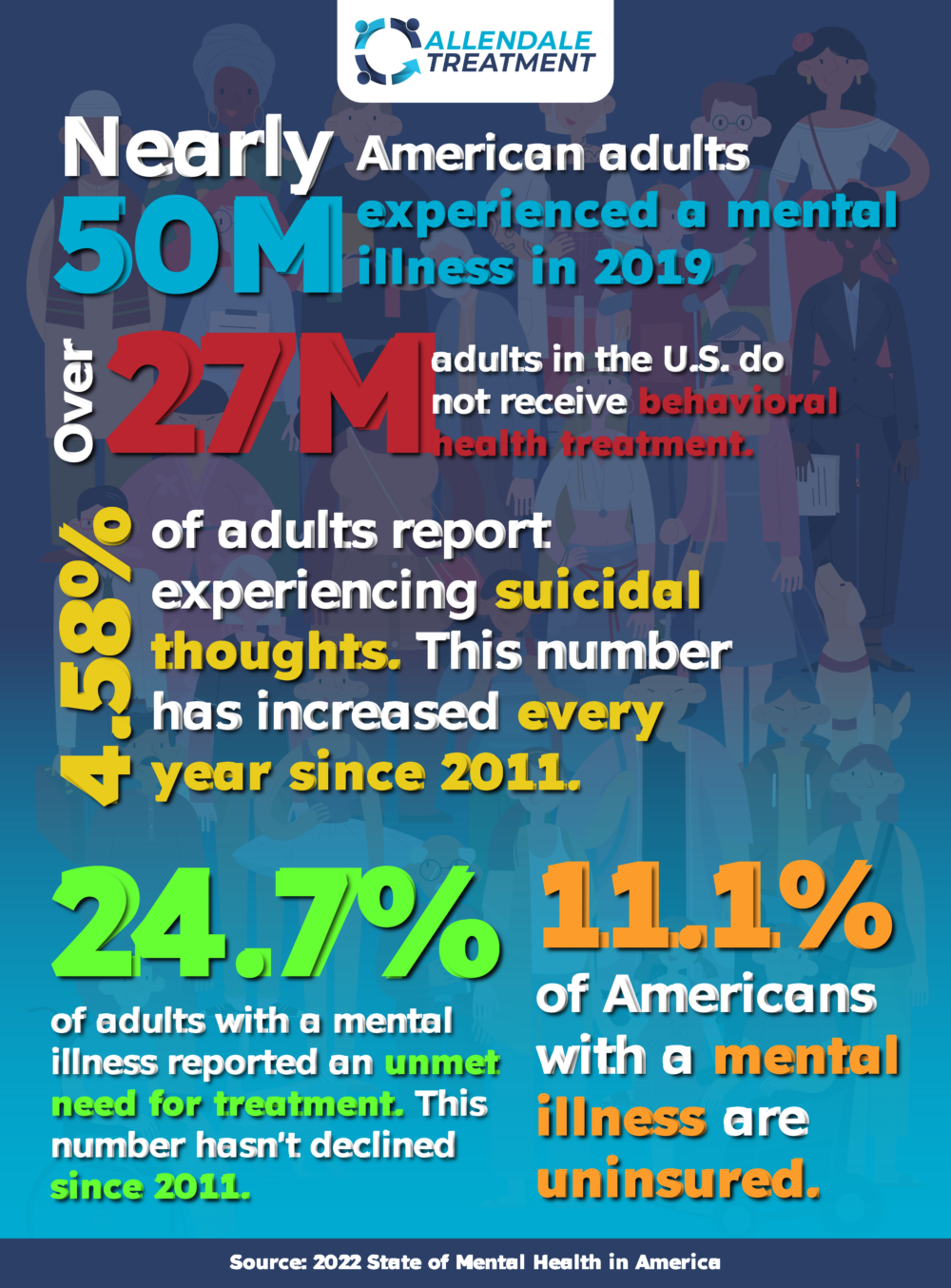
In recent years, many people have struggled with their mental health, in a study conducted in February of 2023 over 30% of adults in the United States reported symptoms of anxiety and/or depression.
Updated: 2023
Written by: Allendale Treatment
If you or anyone you know are struggling with addiction, call (833) 338-6946 to speak with a professional.
Substance use and death rates due to substance use disorders (SUD)s have also worsened over the last decade with overdose death rates increasing by 50% from 2019 to 2021.
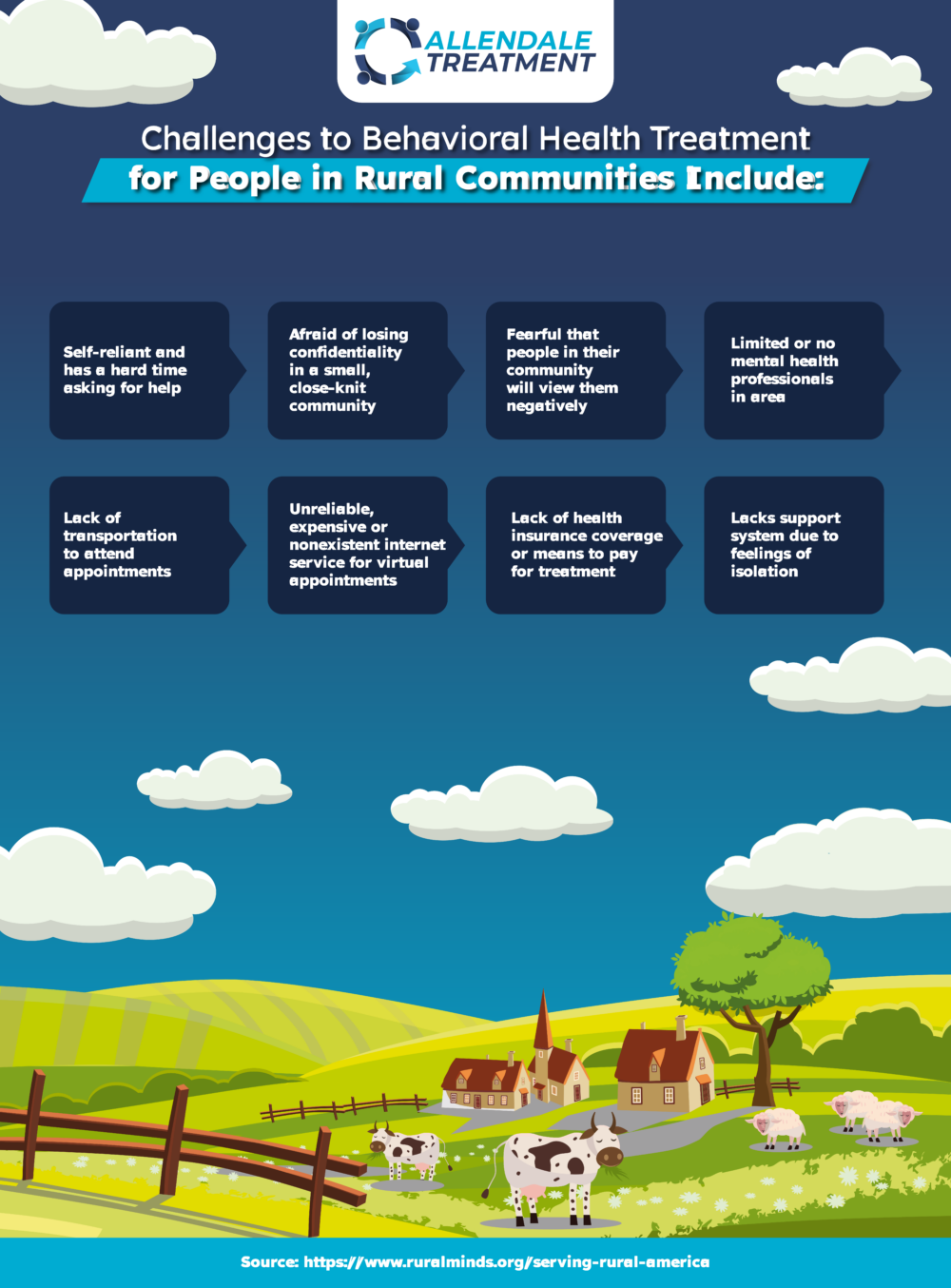
The rise in behavioral health issues and SUDs comes at a time when resources are already strained, and people with mental health diagnoses often face barriers to care. Among adults with symptoms of anxiety and/or depression in 2022 over 20% report needing but not receiving any mental health counseling or therapy. Rural areas that lack access to mental health professionals and minority groups see an even greater proportion of their population lacking behavioral health care.
Rural Communities
Most Rural Communities Lack Behavioral Health Specialists
Americans who live in rural communities have a higher rate of depression and suicide rates of people living in rural counties are 64-68% higher than those living in urban areas. Rural communities also struggle with access to behavioral health professionals and nationally 65% of rural counties don’t have a psychiatrist, 47% lack a psychologist, and 18% lack a behavioral health counselor. Among more remote rural counties, 80% lack a psychiatrist,61% lack a psychologist, and 91% lack a psychiatric nurse practitioner so getting treatment for mental health issues can be challenging.
Rural communities have been hit particularly hard by the opioid crisis with reportedly 3.5% of people 12 and older living in rural areas saying they misused opioids in comparison to the national average of 3.2%. The CDC analyzed patient opioid prescription data from 2014-2017 and found that the percentage of patients prescribed an opioid was higher in rural areas than in urban communities.
People living in rural areas also face unique challenges including feelings of isolation which can deter them from going to detox and rehabilitation treatment facilities for SUDS. Jennifer Christman, the president of the National Association for Rural Mental Health says that isolation can create a downward spiral for sufferers that can lead to even more serious problems. “When someone feels isolated, they feel diminished and apathetic and are unable to pull resources from their own selves,” says Christman. “When it comes to rural mental health, isolation is a particularly dangerous problem.”
Minority Communities Struggle with Access
When it comes to racial disparities, there is a shortage of providers of color in the U.S., in addition to the national shortage of mental health providers across the nation. According to the American Psychological Association as of 2019, 83% of psychologists were White. This lack of diversity might explain why only 43% of US adults with mental health conditions receive treatment and that figure decreases in minority communities such as Hispanic and Latino where only 33% of adults report receiving treatment.
The need for more representation in the behavioral health community is evident with increases in drug overdose and suicide deaths in people of color. In the past 5 years, 43% of Black Americans have experienced an opioid-related death compared to just 22% of Caucasian Americans.
Dr. Rebecca Brendel, who is the associate director of the Center for Bioethics at Harvard Medical School says there needs to be more diversity in the mental health community. “We must diversify, and we must train more diverse psychiatrists and other physicians,” says Brendel. “You have more stress, leading one to suffer negative mental health effects and it is harder to actually seek that help because of institutional and structural racism.”
Technology Can Help Bridge the Gap to Access
With gaps in mental healthcare across the country, technology can help connect patients with the right provider for their behavioral health needs. Virtual or telehealth appointments can be made at the patient’s convenience, improving both accessibility and patient outcomes. For example, before the pandemic ADHD patients in one study missed their behavioral health appointments between 15% to 45% of the time. During the pandemic, this rate fell to 7.5% with the increased adoption of telehealth behavioral health services according to the American Telemedicine Association. Virtual and telehealth appointments can also help reduce the costs of mental health treatment, making it affordable to more people.
Messaging services are yet another form of technology that’s helping to connect people who’re suffering from mental health issues. Clinton Faupel, Executive Director and Co-Founder of RemedyLIVE said that an experience where a listener to his then internet radio show used an instant messaging app to say that he was in distress left an impression on him. “At first I thought it was a joke, but then we found his contact information and notified our local law enforcement to do a wellness check and they found that he was dying,” says Faupel. “I realized that the need to connect with young people who are going through difficult times was evident so we developed RemedyLIVE, a 24-hour chat center. Our goal is to have meaningful conversations around topics like substance use disorders and suicide prevention. We try to approach these topics from a different perspective so that young people are more likely to engage with us when they’re going through a difficult time.”
RemedyLIVE is also partnering with 988, the national suicide and crisis hotline which was created to request support and care for people going through mental health-related crises or for people who are concerned about a loved one. 988 hotline counselors are trained to speak with people in suicidal or emotional distress and handle all incoming 988 calls.

“During the pandemic, the government designated money into 988 to make sure each state could hire the right professionals and find centers that were already focused on suicide prevention. While we’re still waiting on the software to be finished, RemedyLIVE is excited to expand on our reach to help people throughout Indiana who’re struggling with their mental health like other centers and professionals who are associated with 988 are doing throughout the country,” says Faupel.
If you or anyone you know are struggling with addiction, call (833) 338-6946 to speak with a professional.

